Hospitals, businesses, universities and some government agencies are embracing mandatory COVID-19 vaccination policies.
JAN/FEB 2022 | Written by Emily A. Cheslock More
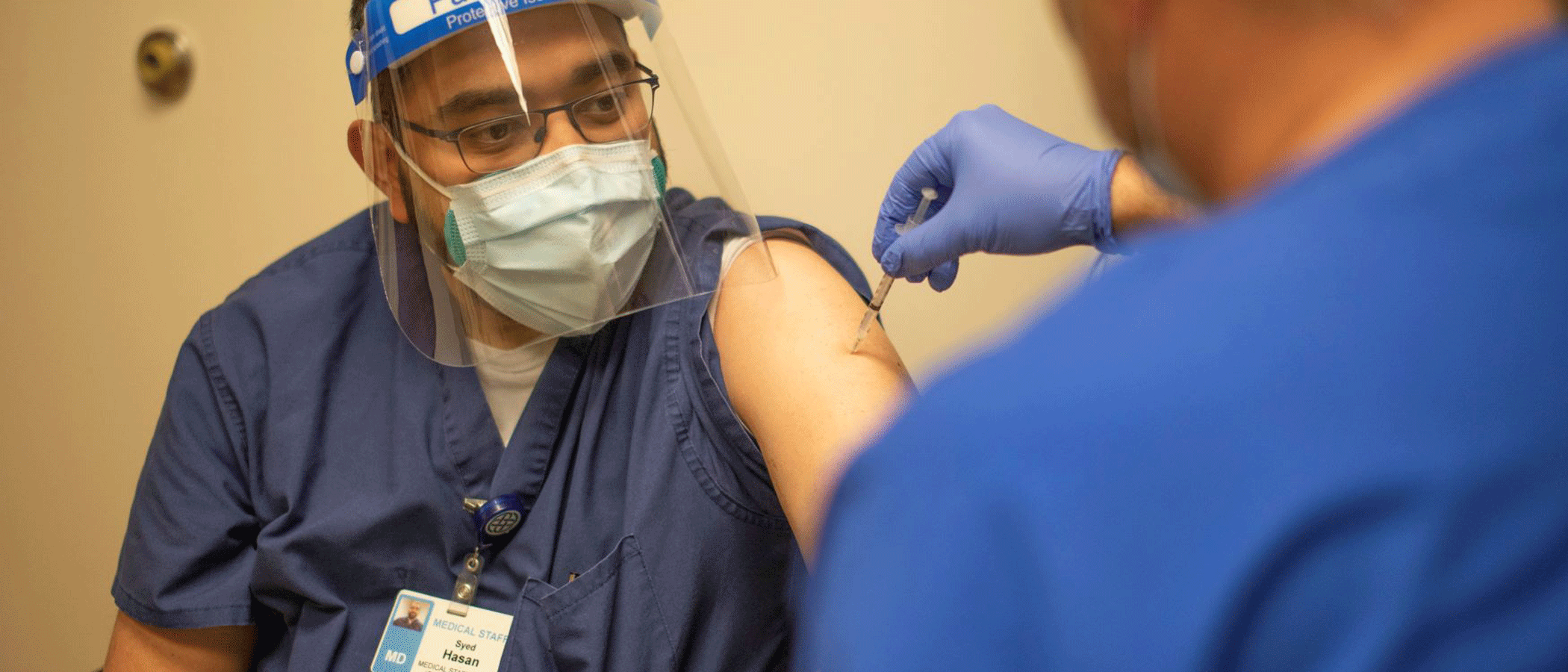
Frontline workers continue their courageous fight against COVID-19. They’ve worked long hours to keep patients alive. They’ve risked their health regardless of hospitals’ precautions to keep employees safe. Behind the scenes, researchers and physicians have worked around the clock to find treatments to protect those who contract the disease from its worst outcomes. Things started looking up in December 2020 when the U.S. Food and Drug Administration issued the first emergency use authorization for Pfizer’s COVID-19 vaccine. Today, we have three available, highly effective vaccines. Pfizer’s vaccine has also been fully approved by the FDA.
“The science proves that the vaccines are not only safe but necessary if we are going to defeat COVID-19. The mRNA technology behind the Pfizer and Moderna vaccines isn’t new or experimental. It’s been around for many years. With more than 300 million doses distributed in the U.S. alone, the vaccines have proven to be extremely safe,” said Marc Boom, M.D., FACHE, president and CEO of Houston Methodist Hospital and chairman of the Texas Hospital Association.
About 50% of all U.S. adults are fully vaccinated, according to data from the Centers for Disease Control and Prevention. The rate of new immunizations began slowing in mid-April, but data show it is on the rise again as COVID-19 surges. According to the Texas Department of State Health Services, Texas ranks 33rd for vaccination, with about 50% of eligible people fully vaccinated.
Some health care workers remain unvaccinated too, despite having priority access to COVID-19 vaccines.
Public health experts worry that outbreaks will continue until a significantly higher percentage of the population gets immunized. The rise in COVID-19 cases brought on by the delta variant is spurring calls for vaccine requirements for health care workers, and some hospitals are listening.
“We have reached a confluence where health care workers want vaccine mandates, and the government is responding,” Ezekiel Emanuel, M.D., Ph.D., a bioethicist at the University of Pennsylvania and a member of President Biden’s COVID-19 Advisory Board, told The Washington Post. “I fully expect more health care facilities will mandate their employees get vaccinated. The nation will be better off for it.”
In June, Dr. Emanuel organized a joint statement from 60 medical groups urging every health facility to require workers to get vaccinated.
On March 31, Houston Methodist required COVID-19 vaccines for all 26,000 employees across their eight hospitals. They became the first major hospital system in the U.S. to do so. Before vaccines were required, they were offering staff $500 bonuses for getting vaccinated.
“The reason we are making the COVID-19 vaccine mandatory is rather simple. As health care providers, we must do everything possible to keep our patients safe and at the center of all we do. Requiring the vaccine was not a decision we made lightly, but science has proven that the COVID-19 vaccines are safe and effective,” said Dr. Boom.
“I fully expect more health care facilities will mandate their employees get vaccinated. The nation will be better off for it.”
EZEKIEL EMANUEL, M.D., PH.D., BIOETHICIST AT THE UNIVERSITY OF PENNSYLVANIA
Houston Methodist is no stranger to leading the way when it comes to staff and patient safety. In 2009, they were one of the first hospitals in the country to require the flu shot. “Mandating the COVID-19 vaccine was reminiscent of how we decided to mandate the influenza vaccine over a decade ago,” said Dr. Boom.
While there was much media scrutiny, the majority of Houston Methodist’s staff was on board. Of about 1,200 in management at Houston Methodist who were required to be vaccinated, only two left the organization. Overall, Houston Methodist had only 178 employees who were not vaccinated or granted an exemption or deferral. Houston Methodist granted 285 medical or religious exemptions and 332 deferrals for pregnancy and other reasons.
“When I was doing my research on the vaccine data with my demographic and age, it was convincing enough for me to decide I was going to get it,” Teal Riley, RN, nursing director for Houston Methodist’s ICU, told the Houston Chronicle. Riley added that she believes the mandate isn’t just about physical protection for staff. “It’s also about curbing the trauma of caring for patients who may not make it out of the ICU.”
As of June 8, Houston Methodist was 100% compliant with their COVID-19 vaccine mandate. Houston Methodist is officially the first hospital system in the country to achieve this goal for the benefit of its patients and staff.
“Since we announced this mandate in April, the media has challenged us. Some outspoken employees even filed a lawsuit. We prepared for this. Criticism is sometimes the price we pay for leading medicine,” said Dr. Boom.
And for employees who decided not to receive the vaccine, Dr. Boom thanks them and acknowledges their contributions and service to the Houston community. “We only wish them well and thank them for their past service to our community, and we respect the decision they made,” he said.
In July, The Department of Veterans Affairs, which runs one of the nation’s largest health systems, announced it would require COVID-19 vaccines for its frontline workers. This comes after four employees succumbed to COVID-19 – all of whom were unvaccinated.
The policy applies to all Title 38 VA health care personnel. This includes physicians, dentists, optometrists, registered nurses, physician assistants and chiropractors —essentially, anyone who works in Veterans Health Administration facilities, visits VHA facilities or provides direct care to veterans. A month later, in August, the VA extended the vaccine mandate to include contractors and volunteers who work in VHA facilities.
“We are seeing the number of COVID-19-positive patients increase as the delta variant spreads. Our frontline medical workers have been through a lot over the last fifteen months. We want to do everything in our power to keep them safe so they can continue treating patients.”
BARCLAY BERDAN, CEO OF TEXAS HEALTH RESOURCES
The U.S. Department of Health and Human Services is requiring all their front-facing health care employees to get vaccinated against COVID-19 as well. The policy will apply to more than 25,000 officials under HHS, including staff at the Indian Health Services and National Institutes of Health who operate health and clinical research facilities or treat patients.
In July, Texas Health Resources became one of the first hospital systems in North Texas to require employees to receive the COVID-19 vaccine. At the time of the announcement, nearly 70% of Texas Health employees were already fully inoculated.
“We are seeing the number of COVID-19-positive patients increase as the delta variant spreads. Our frontline medical workers have been through a lot over the last fifteen months. We want to do everything in our power to keep them safe so they can continue treating patients,” said Barclay Berdan, CEO of Texas Health Resources. “Our first obligation is to protect the health of our community, patients and colleagues at Texas Health.”
Texas Health says that by starting their communications campaign about the vaccine’s benefits back in December, their staff members and community had plenty of information when they announced the mandate.
After Texas Health’s announcement, other hospitals in the Dallas-Fort Worth area also began releasing their plans to require vaccines. Baylor Scott & White Health System, Methodist Health System, Children’s Health and Cook Children’s hospital are now requiring staff receive COVID-19 vaccines.
Parkland Health & Hospital System made plans to require its employees to get vaccinated as soon as the FDA fully approved the shot. In anticipation, Parkland alerted staff that they must receive their first dose by Sept. 24 and the second — or single Johnson & Johnson dose — by Oct. 15. JPS Health Network in Fort Worth will also require employee immunization now that the vaccine has full FDA approval.
“Our Medical Executive Committee voted unanimously to make the vaccine mandatory. I heard the voice of my own primary care provider to make the vaccine mandatory, and I heard patients, coworkers and families that expressed their opinions. We must use all the tools available to us to fight [COVID-19],” Robert Earley, president and CEO of JPS Health Network said in a press release.
Texas Children’s Hospital will also soon require COVID-19 vaccinations for its employees. According to a memo sent to the hospital’s staff, “employees must receive a first dose of the vaccine by Sept. 21 and be fully vaccinated no later than Oct. 19.”
Texas Children’s is the fourth Texas Medical Center hospital to require COVID-19 immunization. Memorial Hermann and Baylor College of Medicine have also announced their immunization requirements. Baylor St. Luke’s will also require vaccines in their 16 hospitals across greater Houston, the Brazos Valley and East Texas.
“We see the impact of the very aggressive delta variant, a significant spike in new cases and hospitalizations, and about 50% of Houston’s population remains unvaccinated, which means the community continues to be at risk,” David Callender, president and CEO of Memorial Hermann, wrote in a press release about their COVID-19 vaccine policy.
Mandating vaccinations is not a new concept, but the debate surrounding vaccine requirements is charged by politics and social factors. Not long ago, flu vaccines were voluntary for hospital staff. Today, 17 states require flu vaccines for health care workers. Schools and universities also require vaccines for students such as immunization against meningococcal disease and measles, mumps and rubella.
One of the first nurses to receive the COVID-19 vaccine at Baylor St. Luke’s Patients Medical Center in December 2020.
No federal vaccination mandate has been tried in court, and none has ever been issued for the general population. Instead, much of the power to mandate vaccines rests with state and local governments following Jacobsen v. Massachusetts in 1905, in which the U.S. Supreme Court upheld a city board of health law requiring all adults to receive smallpox immunization.
There is no clear-cut federal policy for the vaccination of health care workers. While the U.S. government can mandate vaccines for their employees, they cannot order state or local governments or private employers to require vaccines.
“This is not coercion. [Houston] Methodist is trying to do their business of saving lives without giving [their patients] COVID-19. It is a choice made to keep staff, patients and their families safer.”
U.S. DISTRICT JUDGE LYNN HUGHES
The U.S. government also cannot prohibit private businesses from requiring COVID-19 vaccines, the Department of Justice concluded in a recent opinion. At the time of this writing, 11 states have banned vaccine mandates.
In Texas, Gov. Greg Abbott signed an executive order barring COVID-19 vaccine or face mask requirements from government agencies and municipalities statewide. He states that “protection against the virus should be a matter of personal responsibility.” The order also extends to any business or organization that receives grants from the government.
However, private entities can mandate vaccinations among staff. In June, U.S. District Judge Lynn Hughes dismissed the lawsuit brought by a small number of employees at Houston Methodist, saying the requirement broke no federal law.
“This is not coercion,” Judge Hughes told NPR about his ruling. “[Houston] Methodist is trying to do their business of saving lives without giving [their patients] COVID-19. It is a choice made to keep staff, patients and their families safer.”
Publicly funded hospitals cannot mandate vaccines, although several have sought exemptions. The University of Texas Medical Branch in Galveston requested an exemption to require COVID-19 vaccines for staff, but the state denied the request. According to The Dallas Morning News, John Zerwas, M.D., the University of Texas system’s vice chancellor for health affairs, recently raised the exemption request with Gov. Abbott, who was unwilling to change his position.
Several Texas public schools are also hoping to obtain exemptions – with some like Austin, Houston, San Antonio, Fort Worth and Dallas Independent School Districts going against Gov. Abbott’s order and requiring students and faculty to wear masks in the upcoming school year.
At the time of this writing, calls are growing for Gov. Abbott to loosen the rules against mandates — which are currently at odds with the latest federal guidelines. The CDC recommends that even vaccinated people wear face coverings indoors where cases are surging, a step that would protect themselves and others who are immunocompromised or unvaccinated.
Paul Klotman, M.D., CEO and executive dean of the Baylor College of Medicine in Houston wrote the following an April 2021 opinion piece about the importance of vaccination. “As a health center responsible for protecting patients, health care workers and learners, we should have the right to require our employees and students be vaccinated and wear masks unless they have a medical or religious exemption. The reason why? To protect the people we serve from infection by us.”